
DIY lean transformation at Barcelona's Hospital Clinic
FEATURE – You don’t always need a lot of external help to initiate a lean transformation: the experience of the Emergency Department of the Hospital Clínic of Barcelona shows it can be done with very little support from the outside.
Words: Dr Miquel Sánchez, Head of Doctors, and Montse Suárez, Head of Nurses, Emergency Department, Hospital Clínic of Barcelona
People often assume that change will come in the form of a big IT system or a group of consultants walking into the organization and starting telling them what to do. What we have found in just a few months here at the Hospital Clínic of Barcelona is that change can come from very simple improvements, and with very little external help, so long as people are involved.
It was October 2014 when we decided to embark on a lean journey, starting from the most problematic of our areas, Level 3 of the building that houses the Emergency Department.
Some 55% of ED patients are seen on Level 3, which is therefore the floor in which most of our issues concentrate. It just seemed like the most logical place to start our lean experiments.
We decided to do it involving people right away, as we knew it wouldn’t work otherwise. As a first step, we organized a number of one-day workshops to which staff could participate if they wanted to (making them mandatory would have easily been misinterpreted).
We were surprised when 70 people showed up to learn more about lean.
With the help of a number of participants we soon drew our very first value stream map for Level 3, beginning to measure our processes. We then tried to put together our first A3, which gave us the proposed countermeasure that we are currently trying out.
We are planning to introduce the new standards of work at the end of this month [September], and we are currently selecting project leaders and running a number of experiments with countermeasures (so that we can perfect the standard). We are also experiencing “contamination” to other areas: we are analyzing the big bottleneck in our Observation Area (around half of Level 3 patients end up staying for observation), for example, and trying to identify potential solutions. Perhaps we will even sync the Observation Area project with the rest of our initiative.
LEAN EXPOSURE
We both attended the Lean Practitioner Program at the Instituto Lean Management, and came back with a changed perspective. It wasn’t the first time we had heard about lean, but it definitely was the first time we actually studied it.
This is not a first for the ED either. The department had tried to introduce the methodology back in 2011 (still in Level 3) but staff hadn’t gotten on board and the project had derailed. What changed this time around is that both of us believe in the project, and we were able to get people to believe in it too. As Head of Nurses and Head of Doctors, we have to show people how much we believe in the potential of lean principles. If we don’t, the chances of them buying into them are next to zero.
We really think that the only way to apply lean is by involving your internal resources. In many hospitals the lean facilitator is an engineer coming from outside the organization, and it is common for staff to have big doubts about this person and the knowledge they can bring in. We don’t have that here, because we are the people helping to make change happen and we have all the knowledge of the system that is required. You can’t change something that you don’t know.
Oriol Cuatrecasas of the Instituto is of great help. He comes in every once in a while to see what progress we have been making, but it is great to be able to try things out for ourselves, make mistakes and learn from them.
ED staff is now realizing that working together and in flow is the only way to make the system better, and to improve both the patients’ and the workers’ day.
THE CHANGES TO THE PROCESS
The process we are looking at (a patient going through Level 3 of the ED) used to take up to 300 minutes.
We gave ourselves the goal to reduce that time to 160 minutes, and quickly realized that the only way to achieve that would be through teamwork, especially between nurses and doctors.
Thus, we introduced doctor-nurse working teams. When we started to work together to remove the parts of the process that don’t add value, waiting time began to drop.
There were two steps of the process that were particularly critical, and so blatantly wasteful: in one the nurse waited for a doctor to show up for 65 minutes, in the other it was the doctor who waited for a nurse for another 65 minutes. Whenever he or she couldn’t find a nurse right away, they would understandably decide to move on to the next patient. After a few hours, nurses were asked to provide charts for four or five patients at a time, because there were four or five “cases” open simultaneously. Work quickly piled up. In the end, the doctor got all the charts in one go and had to sort through them at the end of the day. It was completely crazy, with bottlenecks and waste throughout! Now that we have the working cells, everything is different – communication is quick and straightforward, and there is no waiting.
We tell our people that patients are always the most important thing, but it is also important to rationalize the way we work, so that we can perform more value-added work.
The new standard for seeing patients that we are trying out at the moment has already shown great promise. The process is more streamlined, people are working in teams, and patients are seen more quickly.
GREAT RESULTS
We have not been able to achieve our goal of 160 minutes yet, but we have managed to get to 180 minutes – more importantly, we got to 180 minutes for 90% of our Level 3 patients. The stability of our results makes us very hopeful.
The greatest achievement of all, however, is people engagement. Staff is asking to try the standards for themselves, and 180 people have now gone through the lean workshop (we started with 70 people out of the 320 employees working in the ED, and we now have a waiting list).
Our plan for the future is to spread the lean word to the rest of the Department, first in the Observation Area, then on Levels 4 and 5, then on Level 2. And then, of course, we will keep improving.
The most critical lesson one can learn from our experience is that hospitals don’t need a lot of resources or to call in a team of external experts to embrace lean thinking. So long as you own the transformation as a leader and involve your people from day one, you will be able to do it by yourself – perhaps with a tiny bit of help from the outside.
We feel very good about lean at the Clinic, and we can see the contagion has begun. We managed to create curiosity, that’s how we know that we will succeed.
THE AUTHORS


Read more


FEATURE – A school board in Holland is discovering the potential of lean thinking and improving its processes to tackle the overburdening of teachers.


FEATURE – The benefits of establishing a lean operating system will support the growth and success of a business in the long term, says Karen Gaudet looking back at her experience at Starbucks.


INTERVIEW - As the use of lean continues to grow in the service industry, questions abound on how this sector can use the principles and practices effectively.
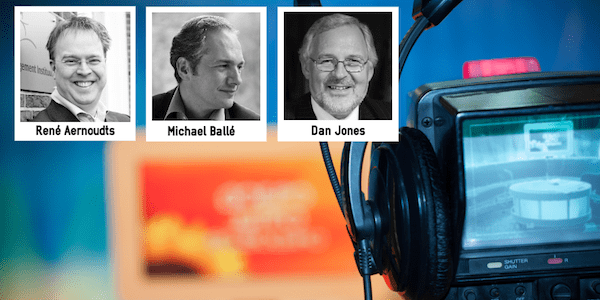

INTERVIEW - In this video interview, René Aernoudts, Michael Ballé and Dan Jones answer a few key questions on what's next for the lean movement.

