
Lazy leadership and ethical decline
FEATURE - Learn how complacent leaders and poorly designed systems can compromise ethics, quality, and sustainability in healthcare organizations
Words: Carlos Frederico Pinto
First published on www.saudebusiness.com on March 17, 2025
I often kick off my presentations by discussing Dr. Deming's Theorems 1 and 2. They state respectively: “Nobody gives a damn about results,” and “A bad system will beat a good person every time.” But what did he really mean by that?
There are many paths to finding an answer. I'll stick to what I used to close my previous article, in which I asserted that it's a leader's obligation to provide opportunities for teams to do their work well, in a fulfilling and creative way.
LAZY LEADERS DON’T ACT THAT WAY
What constitutes a "lazy leader"? This term was coined by American Army engineer and psychologist Leonard Wong, when he addressed the problem of ethical decline within the military.
Military personnel have long understood that, in a war, moral and ethical values are as, or more important than, proficiency with weapons or complex technologies. In fact, American Marines also coined the term "soft skills" (social and behavioral skills related to team performance), in contrast to "hard skills" (skills in handling weapons, ammunition, explosives, or piloting an aircraft).
While studying ethical decline in the army, Dr. Wong observed that it begins with small deviations, minor things, like filling out a form by distorting data – for example, guaranteeing you won't drive an army vehicle over 75 km/h. But in short order, this becomes "commonplace," something "everyone does" that "doesn't really matter because nobody reads it anyway."
Wong identified that, due to numerous procedures and a large amount of bureaucracy in the armed forces, people, tired of so many protocols, find ways to bypass or deviate from these activities. Gradually, small deviations here and there morphed into important but completely unrealistic reports, disconnected from reality, creating misinformation, risks, and unnecessary costs.
Lazy leaders like to find solutions in forms, reports, and bureaucracy. And when faced with a problem or poor performance, they suggest developing a new control process similar to the bureaucratic procedures Wong observed.
When we look at our hospitals, we see the same problems: an excess of irrelevant forms and processes, whose metrics bear no relation to reality or what's truly important. Nevertheless, they consume all of the working time of our already overwhelmed people.
The lazy response to a problem is to create a new process, another daily control item, which only overloads teams but provides no information. It's just noise. That's assuming it doesn't produce unexpected and harmful effects on the gamification of results, to the detriment of patients (recalling that complex adaptive systems are somewhat counterintuitive and frequently produce this type of result).
In the UK's National Health Service (NHS), one of the oldest and largest in the world, ambulance calls were classified by risk, determining priority: higher-risk calls (Category A) had to be attended within 8 minutes. Others could wait longer, between 14 and 17 minutes.
With limited infrastructure and variables like call volume, distance to destination, and traffic conditions, the ambulance service couldn't efficiently handle calls. The system should have been reviewed and redesigned, but that wasn't what was proposed. Instead, they simply created a way to incentivize good performance.
When this happens – that is, when the system imposes impossible goals – people game the system. Or as Isao Yoshino said: "If you always demand success, people will lie to you!"
So, what did the ambulance management teams do? They sought alternatives to meet the target and not lose performance points, which could impact their earnings. Some resorted to obvious workarounds, like retroactively correcting the priority level, creating a large and improbable peak of service precisely at the 8-minute mark, the time limit for high-risk calls.
Others defined the risk category of calls based on relative distance or traffic conditions, leading to almost all high-risk events occurring within a certain radius of the ambulance dispatch center.
Personally, I’m tired of seeing leaders solve their poor financial performance problems by entering meetings with other leaders with a simple and brutal question: "How many people will we have to lay off to meet the midterm’s target?" or "How many patients will we have to admit to the emergency room this month? How many CT scans? How many MRIs?"
Leaders who vilify the work and conduct of their people for a financial bonus don't believe they're doing anything wrong. However, this destroys their people’s pride in doing their job well, degrading the good work and qualifications of their professionals. At no point do these leaders discuss how to improve quality to optimize operational performance.
The path from minor deviations to suffocating bureaucracy, and ultimately to the ethical collapse of an organization’s culture, is paved with small lies, willful blindness, and growing tolerance for misconduct. At the end of that road lies total disregard for the fact that the business game is not just about profits; it plays with people’s lives and well-being, whether they are customers, patients, or employees.
Returning to the problem of the system that, good or bad, will always win – because every system is organized and operates to achieve its explicit or veiled purpose – many organizations have inspiring missions and visions, but not so virtuous practices. Healthcare systems and organizations whose purpose is not related to patient well-being and that lack a long-term vision in this regard are exposed to ethical decline as they try to meet their goals.
Short-term vision, focused on current performance, without reflecting on the impact of periodic layoffs, creates a short-term-oriented culture, which will encourage people to behave accordingly. "Since I know I'm expendable, dismissible just to meet a financial target, I play the game." And this culture leads people to adopt practices like circumventing rules, rushing through mandatory training while staying glued to social media, and neglecting relevant safety procedures. People know they won't be around when the problem emerges, anyway. It's always a short-term project. As Dr. Deming would say, “nobody gives a damn.”
Robust systems have a clear vision and develop long-term relationships and plans aimed at creating value for their customers and generating fair returns for the organization, its shareholders, and employees – which ensures the sustainability of the system itself in the long run. These organizations understand that good short-term results do not guarantee good long-term results.
Perhaps all this explains why many large healthcare corporations in Brazil today have their market value reduced to 30%, or even less than 10%, of their original value. Nobody cares.
THE AUTHOR

Read more


FEATURE – The author explores methods to expand your flow “sweet spots”, enhance focus, and achieve a state of effortless productivity.


FEATURE – How do you ensure that visual management doesn’t become anything more than a way to reassure the boss, rather than foster a learning and problem solving culture? The author reflects on her company’s journey towards effective visualization.
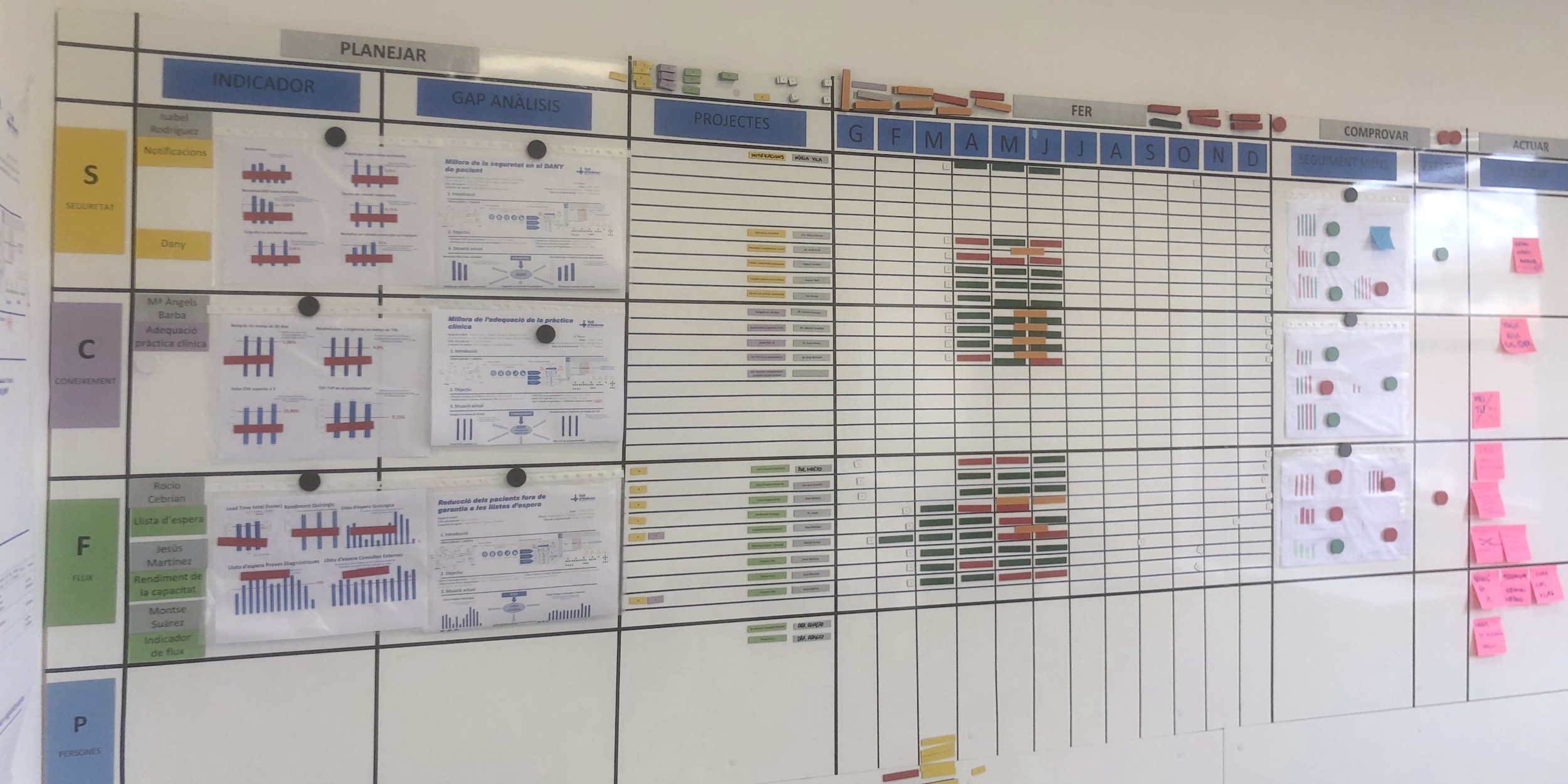

CASE STUDY – Catalonia’s largest hospital is undergoing a successful transformation – supported by pioneering hoshin experiments – that has already turned it into a poster child for lean healthcare in the region.


INTERVIEW - What lies at the core of kaizen activity? How has the concept of kaizen evolved over time? Planet Lean’s editor Roberto Priolo discusses these and other topics with kaizen expert Mark Hamel.
Read more


FEATURE – Healthcare’s complexity demands simplification. By reducing variation, eliminating waste, and rethinking processes, leaders can improve performance, capacity, and safety while enhancing staff engagement and delivering unexpected positive outcomes.


VIDEO - The CEO of a cancer center in Brazil gives us a tour of the their obeya room, taking us through their strategy deployment and explaining how it supports their mission of reducing the burden of cancer.


CASE STUDY – This primary care unit in Brazil is hoping to become a model for other units in their system. Take note, this is how Lean Thinking can spread across healthcare systems.


WEB SERIES – Today, we launch a new documentary series on lean around the world, with the first season focusing on lean in Brazil. In the first episode, we visit the lean clinic on a mission to reduce the burden on cancer in our lives.

