
Putting “loving care” at the heart of a lean transformation
INTERVIEW – PL sits down with a consultant and a manager from the St Elisabeth hospital in the Netherlands to talk about the organization’s “loving care” approach to treating patients.
Interviewees: Rita Arts, care manager, and Marloes Hendriks, senior lean consultant, Elisabeth Tweesteden Hospital
Planet Lean: Can you introduce your hospital to Planet Lean readers?
Marloes Hendriks: The St Elisabeth Hospital is located in Tilburg, in the south of the Netherlands, between the cities of Breda and Eindhoven. The organization employs 3,500 people. We are currently in the middle of a merger with the TweeSteden Hospital, and together we have 1,032 beds and employ 5,500 people.
The hospital (which specializes in traumatology, neurology, and neurosurgery) records about 85,000 admissions and 650,000 outpatient visits every year, while the visits to our ER department total 60,000.
PL: Tell us about your lean journey, please.
MH: We started about 10 years ago. We never made the decision to introduce lean; it just happened. There were a couple of departments - the Microbiology Lab and the Neurosurgery Ward - that had started experimenting with lean thinking. From there, the use of the methodology grew organically and spread across the hospital.
Lean is part of our strategy these days, and everyone is aware of it – I would say that 80% to 90% of our people work or at least interact with lean on a daily basis.
Rita Arts: People are exposed to the use of lean tools across all our departments, and we really strive to facilitate the development of a continuous improvement culture everywhere in the hospital. The implementation of lean is not limited to the wards, but also spreads to administrative departments like HR and Finance.
PL: When did lean get enough visibility that leadership was convinced to include it in the hospital’s strategy?
MH: It happened fairly quickly, around eight-nine years ago. Managers like Rita, for example, regularly participate in “weekly watches,” during which they discuss improvements with different departments. (A weekly watch is pictured in the image above.)
Members of the board go on gemba walks as regularly as possible, too. We are currently trying to bring more consistency to the way they commit to the lean cause, and their involvement is certainly increasing. They promote lean, they advocate for it, and they are proud of what we are achieving – but changing behaviors is really difficult.

PL: How did you get around initial resistance?
MH: We tried to focus on those departments that were most eager to embrace lean and translate its teachings to their people. It was more push than pull, to be honest, but I think that is fairly normal when you start off. You will always have a mix of enthusiastic and reluctant people.
We also found that focusing on people’s daily problems, whether big or small, is extremely useful in fighting resistance.
RA: Specifically, we want people to focus on what they can improve in their work every day, without necessarily relying on external help. The idea is to empower them to do it themselves.
PL: Was there a specific professional group within the hospital with whom you got more traction as you tried to introduce lean?
MH: Not really. I would say that the group of lean supporters has always been quite diverse. For example, there is a group of doctors who really are enthusiastic promoters of our lean efforts, ambassadors even. They are very important to us. But we also have nurses, heads of departments, and team leaders on our side. It is great to see so much commitment from so many areas of the hospital.
PL: You have a concept you really live by at St Elisabeth, called Lean en Lief in Dutch. What does it mean?
RA: The best way to translate lief in English, in the context of the hospital at least, is loving care. It is about the relationship between the professional and the patients – we have found it is critical to have a relationship with the people we care for and be aware of each of their individual contexts. Therefore it is important that professionals stay focused on the patient’s perspective and needs when they provide their care.
People spend a very small part of their lives in hospitals (thank goodness!), and an extra effort is required to fully understand each patient’s personal story and therefore provide better (and better informed) care.

PL: In practice, how does this concept translate into the actions performed by doctors and nurses? Do you have guidelines that people can follow?
RA: It happens in a lot of different ways. For example, say we have a patient who just had hip surgery. For this type of procedure, we have a standard and a clinical pathway that we follow. But if that patient is 75 years old and also suffers from heart disease, they will not fit into that same standard. This means that we need to take into account every piece of information on each individual patient to provide personalized care.
MH: We look at our patients as people, not diseases or treatments. It is all about empathy in the end, and we try to adjust standards to each patient’s situation.
It is a really hard balance to strike, but we are doing our best because it is very important to patients, who are often scared and vulnerable when they come to the hospital.
There is something else to say about the relationship between lean and lief: lean is all about maximizing value for the patient, and we try to involve the people we care for in the improvements we introduce, asking them to give us suggestions and ideas.
RA: That’s right. We ask patients what their wishes and expectations are, and this helps us to get a fresh perspective on the processes we are trying to change. This goes hand and hand, of course, with our drive to care for people in a more loving way and to provide greater value to them.
PL: How has the hospital changed since you introduced this approach?
RA: I have worked in this hospital for over nine years, and I remember that when I first started working here patient questionnaires often told us that people found our doctors to be very arrogant. Today, people tell us how much the atmosphere has changed and that they feel at home and safe when they come here.
MH: When it comes to improvement, I think this hospital has been very successful. We understand that the nature of lean is iterative, and we are not scared to try new things. We run small, quick experiments and then adjust based on what we learn.
We have what we call an Improvement Structure, which is our way to make improvement a daily component of work by introducing a number of techniques, tools and practices (like kaizen, improvement boards, 5S, A3 thinking, and so on). We try to train every colleague to not jump to a conclusion but to really get to the root cause of a problem.
Training happens just-in-time, meaning that people are taught what they need at a specific point in time. It is one-piece flow applied to learning!
THE INTERVIEWEES


Read more


FEATURE – The future has never looked more uncertain for restaurants and cafes. The authors share a set of practical lean tips that can guide these organizations navigate the storm.


INTERVIEW – As we look back at the evolution of lean management in our countries, the story of Instituto Lean Colombia will certainly sound more than familiar.


INTERVIEW – Ahead of this week’s Lean Global Connection, we talk to one of the speakers, who is trying to create a foundry that is lean from the start.
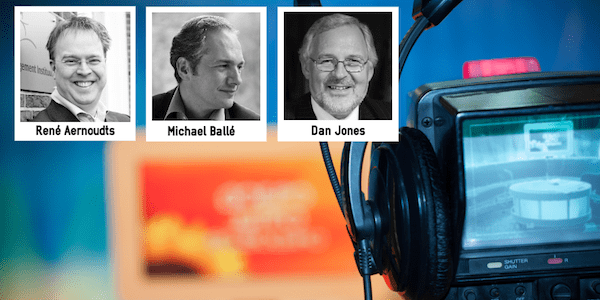

INTERVIEW - In this video interview, René Aernoudts, Michael Ballé and Dan Jones answer a few key questions on what's next for the lean movement.

