Becoming a role model
CASE STUDY – This hospital in Argentina has leveraged the power of Lean Thinking to greatly enhance patient care, even in the pandemic, and receive internationally renowned accreditations.
Words: Dr Javier Sala Mercado, Adjunct CMO and COO, Instituto Modelo de Cardiologia – Córdoba, Argentina
In 2012, when I came back to Córdoba – after almost 11 years in the United States – to work at the Instituto Modelo de Cardiología Privado SRL (IMC), I suggested to the Board that the hospital didn’t need another cardiologist. Instead, I offered to leverage the lean knowledge I had acquired in the US, through research and connections, to help the organization to identify and solve its most critical problems and improve patient outcomes.
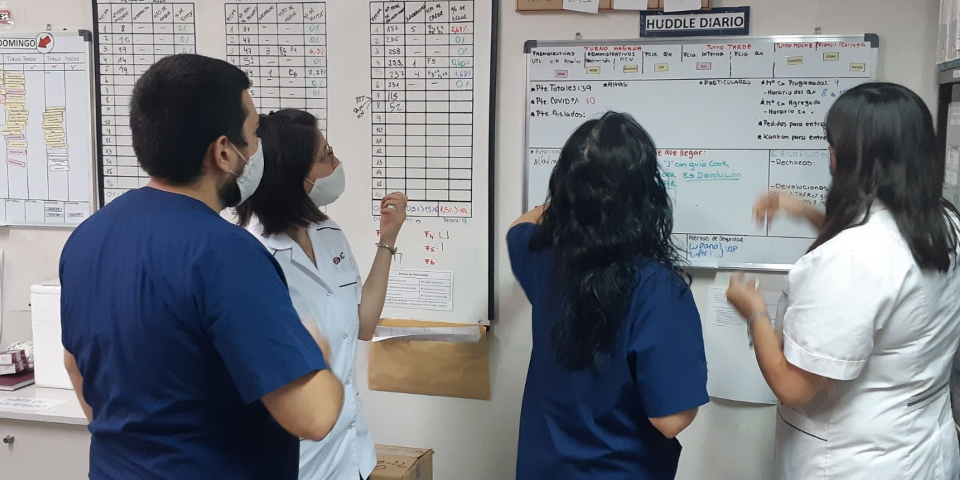
With the Board’s full support and participation, one of the first steps was to reach out to the leaders of the different departments. We wanted to understand how they were managing their areas and what metrics they were using. What we found was that many of the department leaders had no clear idea of their current state. There were hardly any metrics being tracked, and no visual management in place. There was a disconnect between these leaders and their teams and between the department and the organization’s True North. So, to bring visibility of the current state to the various processes in the hospital, we started measuring.
IMC is a 44-year-old “boutique” hospital. In 2019, we recorded 8,703 admissions and 238,000 outpatient visits (of which 57,284 were emergency visits). We only have 72 beds, but with more than 250 physicians we provide a total of 53 specialties. Cardiology is the main one. I knew that transforming a small but complex organization like ours would require patience, especially considering that not all of our physicians are always on site (some are here for as little as two hours a week).
Getting everyone on board would be a challenge, which is why we began our improvement efforts in the areas and processes that seemed to respond most positively to the first timid lean steps we took. Three in particular – our cardiac rehabilitation program, our laboratory and our pharmacy – became our model cells. We started to look into their processes, engaging both local leadership and front-line staff in the improvement work.
Slowly but surely, the changes we made got the attention of other areas and people started to get curious. In those first few years, our transformation efforts focused on the support functions rather than the physicians themselves – laboratory and pharmacy, of course, but also HR, purchasing and administration. We were hoping that improving these areas would capture the imagination of physicians and encourage them to get involved, too.
The first large-scale improvement directly led by physicians was in our operating rooms. In fact, it was them who asked for help. The problem was that surgeons often didn’t know when they were going to operate because it was hard to understand when an OR was available and when it wasn’t. A team was created – which included the Chiefs of Traumatology, Cardiovascular Surgery, Vascular Surgery, Operating Rooms, ICU and Anesthesiology, as well as administrative staff, a board member and myself – and a number of basic lean tools, like value stream mapping, were introduced to bring clarity to the situation.
ACCREDITATIONS AND TRAINING
It had been our desire that the hospital get international accreditations. In 2016, we applied for the Chest Pain Center Accreditation Version 5 with Primary Percutaneous Coronary Intervention, jointly awarded at that time by the American College of Cardiology and the American Heart Association from the United States. It was a huge undertaking for us, but my hunch was that teaching our personnel how to apply Lean Thinking to our processes would help us get there.
Eager to deepen our understanding of lean, we managed to obtain a scholarship sponsored by Cardinal Health (USA) to take a team to the States for a two one-week training sessions at the Academy for Excellence in Healthcare, offered by the Fisher School of Business at Ohio State University. They took place in July and October 2016, and we were the first international team (cohort 9) to participate in the program. The team was comprised of the Chief of Heart Failure, the Chief of Post-Cardiovascular Surgical Care, the Chief of the OR, the Chief of the Cath Lab and myself. To prepare and to get the team familiar with the lean lingo, we read together Managementon the Mend by John Toussaint, as well as the program’s pre-reads.
In many ways, those two visits to the United States were a game changer for the lean transformation of IMC. I had been frustrated with the slow progress and with the physicians’ buy-in we had been seeing and, as usual, the answer was in the gemba. Getting leaders from our hospital to visit other organizations that were further along in their journey – like the Ohio State University Wexner Medical Center in July (at the time, their transformation leader and Chief Quality Officer was Susan Moffatt-Bruce, who was our assigned coach during the training) and Cardinal Health’s main Distribution Center in October – opened their eyes to the opportunities afforded by lean. That’s when things started to come together: on the one hand, we had projects run by support functions across the hospital; on the other, physicians who were finally understanding the value of lean.
From 2012 to 2016, when change was driven by our support areas, the progress we made was great but limited to the different silos and largely unseen by physicians. Even when we transformed the process in the operating rooms, they recognized it but still didn’t engage fully outside the ORs. Things changed after we went to the US, however. That’s when the physicians started to get involved and we began to see more cross-functional projects and the systemic change they are capable of effecting.

As part of our training with the Academy, we successfully completed a project to improve discharge time – a sticky point for hospitals around the world. By introducing flow to the process, we were able to make great improvements: between 2016 and 2017, we achieved our target of 40% of patients discharged before 10:30 AM, 60% before 12:30 PM and 80% before 2.30 PM. (Today, in 2021 our target is to have 50%, 70% and 80% respectively.) Our work was documented in a White Paper.
Proving we were on the right track, in 2017 we received the much-wanted Chest Pain Center with Primary PCI accreditation. It took us less than a year. In 2018, we also got the ACC Heart Failure Accreditation – the only one outside the United States. Keen to build on our progress, we even brought the Academy to Argentina for three week-long teaching sessions and 2 week-long coaching sessions in 2018. This represented another powerful catalyst for change, which created incredible synergies and awareness and greatly deepened our understanding of Lean Thinking.
The key to all these achievements (we also won an ACC First Place award for quality improvement and received the ACC recognition as an International Center of Excellence in 2019) was helping our people to speak the same language – that of Lean Thinking – and pulling forces to work towards a common goal. Ultimately, this has allowed us to also maintain our results over time.
There is no doubt that another fundamental element in our transformation is the support we have received from leadership at all levels (without it, sustaining change is impossible in my opinion). Our approach is based on the idea of continuously training leaders and educating from the top down, and I believe it has helped us to not only get the leadership support we needed to drive the transformation, but also to identify our best change agents.
When it comes to learning from others, we have invited many lean experts since 2014 to come and visit our gemba and spend several days with us at the IMC – including Marcelo Zottolo, Susan Moffat-Bruce and Peter Ward from the US, Myrna Flores from Switzerland, and José Ferro and Frederico Pinto from Brazil. Some of them have given workshops, others have delivered lectures to share their vast knowledge. Going on gemba walks with them and receiving feedback on our A3s was fundamental.
With regards to sharing knowledge internally, word of mouth is still very much our modus operandi. It’s not structured and it’s not what we want but it works, at least until we can standardize and develop our own lean healthcare development programs (which we hope to accomplish this year). It is through word of mouth that we have been able to bring lean from one area to another at IMC – the same idea that is behind our Lean Day, an end-of-year get together when different people present their A3s. We are also very proud to see how our lean efforts are inspiring other organizations: after attending our Lean Healthcare Summit in 2018, the first ever in Argentina, we have seen a number of hospitals in Buenos Aires embark on their own lean journeys.

RAISING THE BAR, EVEN IN A PANDEMIC
An article published in The Economist in October 2018 said that “most economies are ill-prepared for even a mild recession”. We could talk about “economies for hospitals” and the sentence would still make perfect sense. In Argentina, we are sadly very used to economic turmoil: the country recorded an inflation increase of 53.8% in 2019 and of 36.1% in 2020. In 2019 alone, our labor costs also increased by 53.8% and in 2020 by 21.4%. What do you do in a situation like this? Our response was clear: we need to create more value for patients. Like George Merck once said: “We try never to forget that medicine is for the people. It is not for the profits. The profits follow, and if we have remembered that, they have never failed to appear.”
Indeed, this idea has informed our improvement work since the very beginning, whether we were trying to answer our patients’ calls right away or improving the patient flow through ambulatory care. We have achieved great results by continually raising the bar, reminding ourselves that we can always do better and offer the patient a better experience. It’s worth remembering, for example, that while today over 90% of our patients go from reception to blood extraction in less than 10 minutes, our initial target was 15 minutes – in line with the 2016 Cleveland Clinic’s target.
Overall, since 2012 thanks to lean, the Instituto Modelo de Cardiología has achieved – prior to Covid-19 – increases of 31% for surgeries, 68% for admissions, 84% outpatient visits, 103% for ER visits (among other results). Lean Thinking has allowed us to streamline processes, reduce waiting time for patients and improve the quality of our care. Something I am very proud of is the fact that we were able to sustain these results throughout the pandemic, as well.
Over the course of the past year, many of our projects had to be paused, as the fight against Covid-19 became our number-one priority. This is a war, and we haven’t been strangers to loss (in fact, we lost some of our lifelong patients to this virus), but I think it’s also important to celebrate our successes: our in-hospital mortality for Covid patients is 10%, considerably lower than the global average, and in such complicated economic conditions here in Argentina we have been able to keep everyone on payroll.
It has been moving to see our staff come together and leverage their lean knowledge to protect each other and our patients as best they could. For example, we have seen doctors perform some of the tasks that are typically a prerogative of nurses as part of our collective effort to reduce the number of touch points with Covid-19 patients and therefore limit the staff’s exposure to SARS-CoV-2 and optimize the amount of PPE used without decreasing our quality. Since the pandemic began, standardization has allowed us to make a correct use of our stock of PPE in every single corner of the hospital and never run out (in fact, we consumed more in March, when we were early into the curve and only admitted one Covid-19 patient in the entire month, than in the October peak, when we were receiving 150 suspected Covid-19 cases per day). Simply put, I don’t know how we would cope with this emergency without lean.
Lean has been fundamental to our transformation and successes since we started our journey nine years ago. We therefore encourage every healthcare organization in the world to explore all that lean can provide, to improve their processes, patient outcomes and satisfaction of both staff and patients.
THE AUTHOR

Javier Sala Mercado M.D. PhD. is Adjunct CMO and COO at the Instituto Modelo de Cardiologia in Córdoba, Argentina. IMC is where the Lean Institute Argentina (run by Javier) was born and is being developed with the help of Lean Institute Brazil and the Lean Global Network.
Read more


INTERVIEW - As the use of lean continues to grow in the service industry, questions abound on how this sector can use the principles and practices effectively.


WOMACK’S YOKOTEN – The sharing economy came with a very “lean” promise – underutilized resources made available to those who need them for a reasonable fee – but not all that glitters is gold.


INTERVIEW - Thanks to strong leadership support and an effective system to partner with private sector firms, Washington State is proving how successful lean production principles can be in a government setting.


CASE STUDY – There is more to Siena than the Palio: the Tuscan city boasts of one of the most advanced examples of lean healthcare in Italy. We asked the team at the University Hospital how they are doing it.

