How we gradually built our CI model
INTERVIEW – Cleveland Clinic has been on a lean journey for a few years now. In this interview, their Chief Improvement Officer and Chief Nursing Officer talk continuous improvement, metrics, and sustaining results.
Interviewees: Lisa Yerian and Meredith Foxx
Roberto Priolo: When and how did the lean journey of the Cleveland Clinic begin?
Lisa Yerian: In 2006, we created the earliest process improvement team. They were using a variety of tools and approaches, including lean, six sigma, and project management, and largely focused on discrete projects and a few tools. In 2012, we made a commitment to build a culture of improvement. I reached out to Mark Reich at the Lean Enterprise Institute for advice on how to get started, and he told me: “Sounds like you are going to have to do an A3 on that!” I had never made one before, but I got John Shook’s Managing to Learn, studied the A3 examples in it, and got started with my first ever A3 – “How do we change our culture to a culture of improvement?”. The way we aspired to build that culture was deeply rooted in lean methods – including A3 Thinking – from the beginning.
In 2013, we built our first model area in Finance, and then we expanded into Nursing, Pharmacy, and other areas. From there lean has continued to spread across the organization.
RP: When did the CCIM come into the picture?
LY: After the first experiments in our model areas, engagement grew, as more and more people got interested in participating in the lean work. In 2014, we were working with a growing number of teams and realized we needed to be a bit clearer and more concrete about what we were actually doing to build a lean culture. So, I asked the team to start putting our approach down on paper. What they came up with was the earliest version of the Cleveland Clinic Continuous Improvement Model (CCIM).
\nOur model really grew from needs expressed by caregivers in our organization. We had started with problem solving, using A3 thinking to solve real problems each team was facing in their work. As those initial A3 efforts began to yield results, area managers expressed concern that we would start new A3s “on everything”. It became clear that we needed a system to identify and prioritize what problems we should focus on. That became our problem-solving system. But then the managers started asking how they would know what problems should be prioritized. That led to the realization that we didn’t have a clear strategy or hoshin to guide our improvement work, and, eventually, to the introduction of an organizational alignment system. So, basically, we gradually built the different pieces of the model through listening to the experiences and needs of our teams.
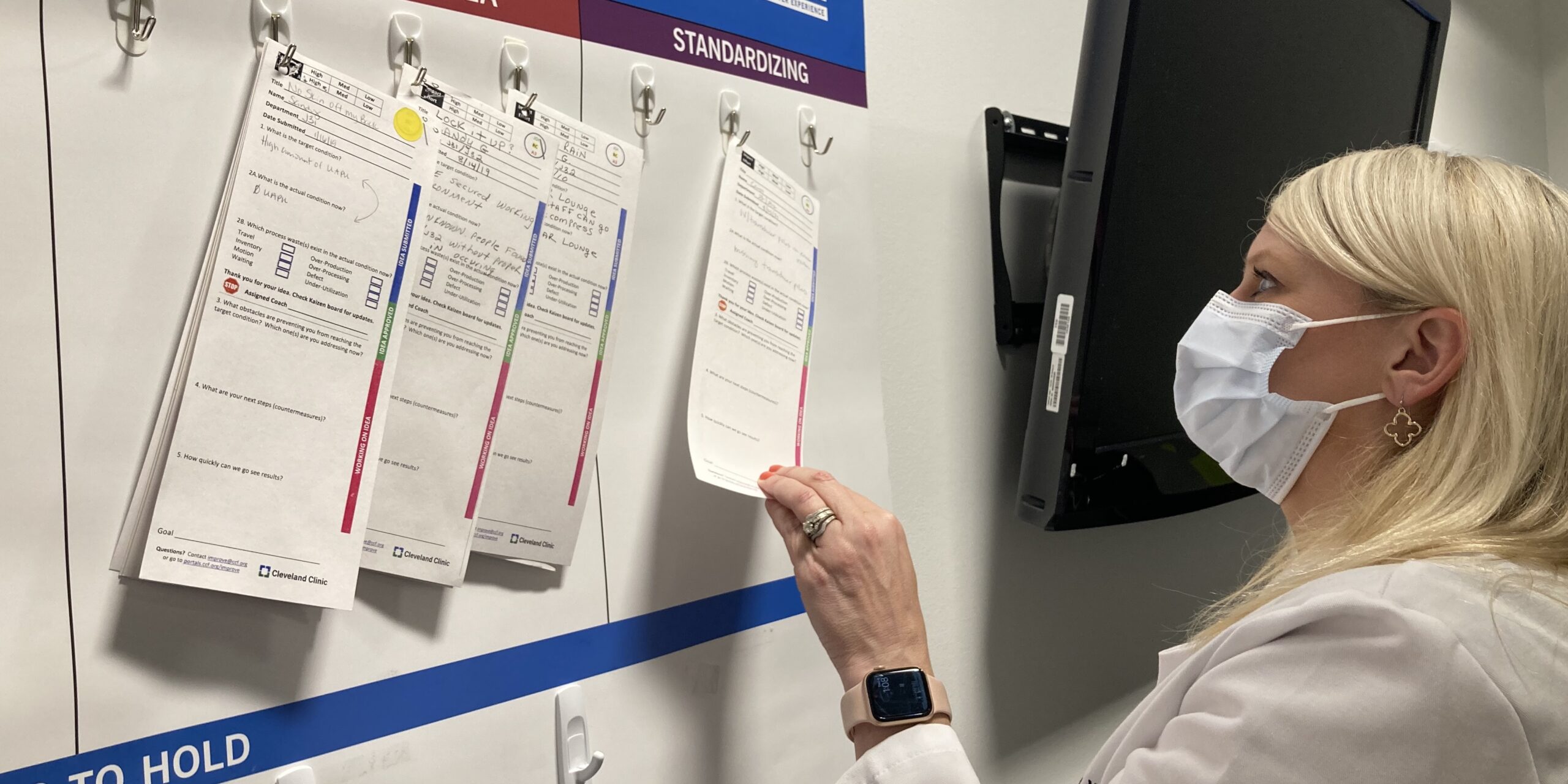
\nAs we went from team to team, we realized that the core questions teams needed to answer to build a culture of improvement were quite consistent: Alignment (“what matters most?”), Visual Management (“how are we doing today?”), Problem solving (“what gets in the way?”) and Standardization (“do we always do it the best known way?”). It is around those questions that we built the CCIM, and they didn’t change. (By the way, our model aligns very well with the Lean Transformation Framework.)
RP: What was the experience of the Nursing Department with CCIM?
Meredith Foxx: We were definitely early adopters. My current nursing leader began using the improvement model to have each of her team members do their own A3s around a problem the department was trying to solve. Our focus is using the CCIM and the standard tools to address what matters most – this is an ongoing process with our own team and then cascades within the nursing teams.
To this day, the CCIM is the model that informs our improvement decisions. We do monthly operating reviews focusing on the OKRs – what matters most – during which everyone reports out on what they are trying to improve and their key results. People are expected to use the methodology to achieve their results.
RP: Nursing is often one of the first areas to start working with lean. Why is that?
MF: Nurses like to fix! If they can provide patient care more efficiently and solve problems, they will. They like to see an evolution and an improvement in the provision of care.
RP: How did you reach the physicians and other areas of the clinic?
MF: Some of the problems we have focused on recently are interdisciplinary and require a team approach. When you start to get closer to the root cause of a problem, you typically find out that other departments or groups of caregivers (employees) are involved. That’s our cue to bring in more people into our problem-solving work, to expand the scope and reach of our projects – the majority of which are still team based.
RP: Metrics-wise, how important has it been to set a clear vision for the organization and how do you connect it to the work that happens at the gemba every day?
MF: Our goal at Cleveland Clinic is clear. We want to be the best place to receive care and the best to work in healthcare, and to always deliver the highest quality and safest care. There are national benchmarks for healthcare organizations, and we are expected to assess our performance based on those metrics. Once we highlight the metrics we are struggling with, we immediately know what our next priority is.
LY: Our goals are centered on four care priorities: caring for patients, caring for caregivers, caring for the community, and caring for the organization. These four elements inform the way we talk about our goals, which is even reflected in the structure of our tiered daily huddles. This approach gives us a way to zoom in on each strategic dimension of our work and identify the problems we need to tackle next.
RP: How has the system supported the improvement of the organization? Can you share some examples?
MF: The first that comes to mind is our sepsis improvement. Sepsis is a life-threatening condition that causes high mortality in hospitals. We analyzed the problem in depth, looking at its root causes and coming up with a set of countermeasures that ended up altering this quality and safety metric significantly year over year. Another project we are proud of concerned readmissions (returning to the hospital for the same reason in a short time frame), in particular those linked to heart failure. That metric, too, has been improving dramatically year over year and now meets or exceeds the national benchmark.
LY: We also determine the financial impact of our improvement work. The combined one-year impact of our improvement work over the past five years amounted to $159 million.
RP: Cleveland Clinic has been on a lean journey for a long time now. What helps you to sustain the transformation and continuous improvement culture?
MF: We have done a good job at integrating the lean culture into our daily leader standard work. It’s been interesting to see how, even during the pandemic, in the areas where lean is deeply rooted, the daily practices that we rely on to ensure high quality and safe care have not skipped a beat. We now know we can sustain our way of working even through challenging times, and I believe that’s because people see the value lean brings to their work.
THE INTERVIEWEES

Lisa Yerian is Chief Improvement Officer at the Cleveland Clinic

Meredith Foxx is Executive Chief Nursing Officer at the Cleveland Clinic
Read more


1 QUESTION, 5 ANSWERS – Without the active participation of people in improvement activities, lean is nothing but theory. Sadly, engaging folks is easier said than done. We asked five lean practitioners to share their approach to people engagement.


FEATURE – In this interesting piece, the author explains how lean provided everyone, everywhere with a framework to work their intuition muscle and develop insights.


FEATURE – Study tours in Japan are an increasingly popular learning tool for lean practitioners. The author reflects on the first ever tour she ran and on what it left people with.


INTERVIEW – Dan Jones will be a keynote speaker at this year’s Lean IT Summit in Paris. In this interview, he gives us a sneak peek of what he is going to talk about.

