The first steps of a Paris hospital towards lean healthcare
NOTES FROM THE GEMBA – On this gemba walk in the cardiology department of a Parisian hospital, the author discovers how the team is changing its internal dynamics and processes to make lean their way of thinking.
Words: Catherine Chabiron, lean coach and member of the Institut Lean France
As I stepped into the Hôpital Lariboisière with Benjamin Garel, Lean Healthcare Director at Assistance Publique – Hôpitaux de Paris (a system of 39 university hospitals in the Ile de France region, caring for eight million people a year and employing 100,000), we were met by a smiling lady who insisted that we try and spot some of the 14 “safety mistakes” she had arranged in a room with a dummy patient, a tray of food, the patient’s file and medication.
This exercise was part of the Safety Week activities organized by the hospital for both staff and visitors – a fun yet effective way to remind people that inadequate prophylaxis, wrong drugs or inaccurate labels all contribute to a poor quality of care, which in a hospital can actually mean serious illness (or even death) for a patient.
Applying lean in healthcare means to get medical staff and management to see problems and pull the andon cord to try and solve them, and to pull flow to learn to navigate a complex environment with silos that are normally ignoring each other. As if things weren’t difficult enough, concepts like “late delivery” or “not right first time” have a very different meaning when the customer is a patient in pain. I have always admired people like Benjamin, who – despite these difficulties – take on the challenge of bringing lean to healthcare organizations (he first did it in a hospital in Grenoble, before going to work for the Assistance Publique – Hôpitaux de Paris, where he is leading a lean transformation).
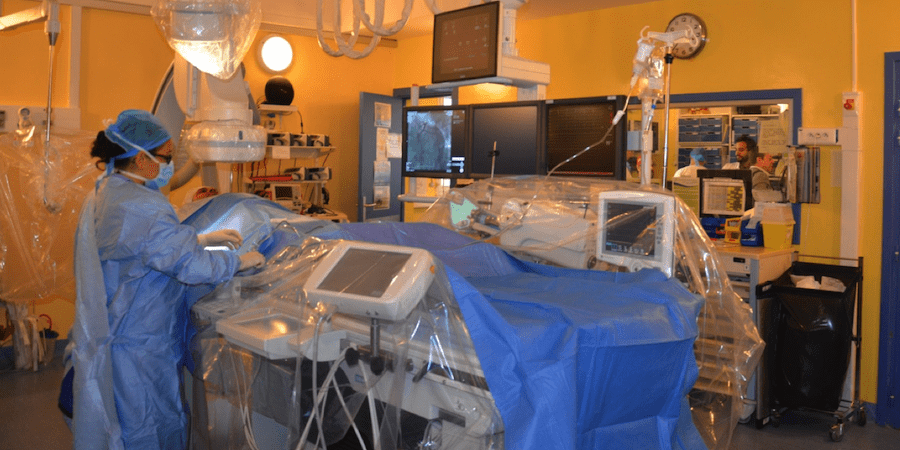
Our destination that day was the Coronary Angiography unit of the hospital’s Cardiology department, headed by Professor Patrick Henry, who decided to use lean thinking to increase patient satisfaction and motivate all team, from physicians to nurses.
Before I tell you about the lean work the unit undertook, let me give you some more background: much like manufacturers and service companies, hospitals in France have to compete with other public hospitals and private clinics on a number of specific services, such as angiography. High competition in a saturated market is a normal part of a hospital’s daily life. At the same time, public hospitals are seeing a demand increase (due to an ageing population, but also because they represent an alternative to practices closing at night or for less well-off people who need to consult a doctor). All of this is made even more complicated by severe budget cuts.
So, let me tell you what was happening at the Hôpital Lariboisière before Patrick Henry decided to start a lean journey with Benjamin’s support.
Most patients come to the angiography unit for a check-up, but if their coronary arteries are in a bad state, the routine check can easily turn into a procedure, like the dilation of an artery and the placement of a stent (a mesh tube that prevents occlusion). Patients who need to undertake such procedures have no time to waste, as they are usually at high risk of coronary thrombosis – commonly known as a heart attack: this means that, as far as lean goes, heijunka (the levelling of the production workload) doesn’t apply here and the team has to cope with whoever comes their way.
When patients came to the unit from outside the hospital, they would all be given an 8am appointment on a certain date. They would all flock in at the same time, nervous and hungry (they have to be on an empty stomach) – having to wait for the administrative file to be completed and for the nurse to prepare them, which includes shaving them, running tests and, in some cases, pre-medicating them.

As always when we batch, the last patients to go downstairs to the angiography ward for their check would wait for hours in the outpatient area – if not the whole day – with no indication of when they might be called down, and no food. By midday, they’d usually be nervous, angry, shouting and cursing, which inevitably impacted the stress levels of the medical staff. Nurses from the Day Hospital (outpatient area) would call up their colleagues from “Coro” and shout at them, to which they would normally reply something along these lines: “We can’t do any better. The third patient turned out to be a difficult case requiring three stents. We haven’t even had time to sit down and have a bite to eat.”
The discussion on lean created a sense of awareness that something could be done to improve the situation and that patients would perceive the quality of the overall medical treatment (the product) to be higher if its delivery (the associated service and logistics) could be improved. Unfulfilled basic expectations (even when unexpressed) will “kill” a perfect product, just like a dirty restroom in a restaurant will kill the dining experience.
The first step Professor Henry took was to convince the different functions involved in the process (people in charge of the appointments, nurses in the outpatient area, and medical staff in Coronary Angiography) to start meeting regularly and discuss possible opportunities for improvement.
The seed of continuous improvement was planted, which led the teams to eventually change their standard: a daily stand-up meeting at 2pm is now taking place with all parties involved to review waiting times and problems together. The team board displays basic data on the waiting times, and is manually updated during the meeting: this is when success is acknowledged and the gap between the current state and objectives discussed. Each member of the team – whether from the “Coro” ward or from the outpatient area – is free to join in the discussions on problems, while Prof. Henry writes on the board the experiments to be launched or the actions to be tracked. This is not a traditional fully controlled and static board – it is, rather, an open space for team thinking.
Right after the meeting, the team moves to the nurses’ room to plan for the next day, using the common scheduling system. When trying to level the effort throughout the day, the patient’s information and context are taken into account more than ever before. The discussion among all stakeholders over the best schedule was the first breakthrough: outpatients are now given an appointment at different times (levelling arrivals throughout the day), and the average waiting time has dropped by 40% in six months. When lean came into the picture, only half of the patients waited less than five hours for their check-up – now it’s 95%. In certain cases, patients are also allowed to have breakfast.
These changes are now established and they have amazingly improved the atmosphere in the ward. Things are much more relaxed than they used to be, and the collaboration between functions has become obvious. Everybody has accepted the new way of working as a massive improvement.
As always, however, when you start observing and discussing details, you identify a number of open points to which we can apply the lean concept of “reusable learning,” as defined by Michael Ballé, Dan Jones and Jacques Chaize in their Planet Lean article (the risk of limiting ourselves to reusable knowledge is that we will merely “copy and paste” from other experiments without thinking much). To facilitate thinking along these lines, Michael, Dan and Jacques suggested the use of this grid:

If we pick up some of the activities in the left column, we are quickly able to re-frame some of the problems the “Coro” team is experiencing, which are regularly discussed in the stand-up meetings:
- Reduce batches and increase the frequency of pickups: In case a patient arrives late (or doesn’t arrive at all), the same time slot is given to two patients (even though this is still batching). The outpatient nurse finds herself overloaded in the early morning (to prepare everything) while the “Coro” staff awaits (or moves on to other tasks). Waiting time has improved but the average is barely below three hours, which is still too long for patients.
- Move closer to continuous one-piece flow and just-in-time: as the outpatient nurse prepares the patient, she wonders what level of testing she should target – depending on the intervention, she has an array of tests to run and risks to check the patient for. So, just in case an artery dilation is needed, she increases both the number of tests and the preparation time. Far from doing only what is needed.
- Move production pace closer to sales pace: with 10 patients per day on average, the ward would be expected to move to a new patient every 48 minutes. The process duration ranges from 10 minutes for a normal check-up that doesn’t reveal any problems to two hours for procedures, should the angiography reveal that arteries are in bad shape and need immediate “repairing.” There is only one room available, though, which means complex procedures are delaying simpler ones. Additionally, the arrival of last-minute urgent patients can disrupt a well-programmed flow.
- Move detection closer to the defect creation, stop at every defect: great progress has already been achieved in terms of the quality of the work environment (mainly its atmosphere). Still, how do you check quality in a hospital ward? How do you decide when to stop (Jidoka) and ask for help? How do you learn from mistakes?
Bringing lean to healthcare is a long and painful process. Organizations are complex, and people’s well-being is at stake when a company is marred by poor quality or efficiency are there. You cannot select the patients you prefer (this is public service), nor streamline your lines of products to focus on what you know best or where you have managed to create for yourself a competitive advantage (private clinics can, but not public hospitals). Openness and transparency when it comes to problems and mistakes remain difficult topics of conversation in healthcare, because of the risk of legal action. But what Benjamin is learning the hard way, together with all those willing to think in a different way and act accordingly in the hospital, is to accept that there is always much more to learn and, critically, that before anything else we must learn how to learn.
THE AUTHOR

Catherine Chabiron is a lean coach and member of the Institut Lean France. She previously held the role of Director of IS Governance at Faurecia, a large French industrial group, working for eight years at the heart of the IS department's lean transformation.
Read more


CASE STUDY – The turning point in this Colombian construction company’s transformation came when they started to embrace lean as a culture rather than just a set of tools.


FEATURE – In this article, Joakim Hillberg shares his experience teaching trainers how to run lean games and some hints on how to practically and effectively coach game participants.


NOTES FROM THE (VIRTUAL) GEMBA – This week, the author chats with an innovative insurance company as it relies on its lean learnings to ensure business continuity and switch to remote working during the Covid-19 crisis.


COLUMN – As individuals, how do we relate to the Lean Community? And what motivates us to stubbornly continue down the improvement path, often against all odds?

