
Teaching A3 skills to medical students

FEATURE – Problem solving is a fundamental part of being a leader, which is what led this medical school in the United States to include A3 thinking in its curriculum.
Words: Dr Jack Billi, Medical Director, Collaborative Quality Initiatives at University of Michigan Health System
Whether or not they will have decision-making power in their future organizations, our medical students will be required to practice leadership skills throughout their careers. At the University of Michigan Medical School, we believe that one of the most important skills they can develop is the ability to solve problems and to coach others to do the same.
It is with this in mind that, for over a decade, we have run a month-long elective rotation for students that are about to receive their medical degree. The rotation – which is named “Physicians as Leaders and Problems Solvers” – is taken by a little more than 1/10 of the medical school class. We have one to three students working with us every month.
The program begins with the students selecting the problem they want to work on and then receiving A3 training. Throughout the month, they use the A3 model to investigate the problem at the gemba, looking for its root-causes and identifying possible countermeasures they then offer the problem owners in the form of recommendations. Much like the history and physical a doctor performs on a patient who is admitted to hospital (which initiates the problem-solving process and recommends a course of action), the A3-based work the students do is limited to the analysis of the problem and proposing possible countermeasures (a proposal A3).
Another activity in this elective rotation is attending leadership meetings and seeing the behind-the-scenes of how the health system works. Even though they usually find such environments to be quite daunting, I try to encourage them to be thinking about what problem the leadership team is talking about, who owns that problem, what the root causes are, how they are going to monitor the problem, and so on. Dissecting what’s going on in that meeting using their problem-solving skills can be a very useful exercise.
We touch base with the students multiple times over the course of the rotation. Occasionally, they join intensive training through one of our courses – either a two-day or a five-day course on lean thinking. When they don’t, I typically do a short one-on-one A3 training for them. Like Porter and Sanderson do in Managing to Learn, I also have a formal check-in (catchball) meeting with each of them once a week to see what they have learned so far and if they have a plan for what to do next. On the last session of the rotation, in the fourth week, the students present their findings. For this, we use traditional A3 etiquette: every person gets a copy, they present their proposal A3 in 15 minutes, and then we practice humble inquiry.
The problems our students pick vary widely. They range from internal issues in our medical school curriculum to identifying septic patients as they enter the ER, from determining whether patients with liver failure want aggressive treatment or palliative care as soon as they are admitted to how to correctly use a new heart attack test.
Our goal is not to have students actually solve the problem, but to give them deeper exposure in analyzing a problem. Nonetheless, many of the countermeasures end up being implemented. To complete their analysis, the students always work with the problem owners. As a result, their proposed countermeasures are often naturally woven into the real improvement work. Other times, things happen and we don’t even know. A few years ago, one of the students going through our rotation looked at the reasons behind the hip fractures fixed by our orthopedic surgeons. His analysis revealed that the biggest risk factor found among those patients was having had a fracture previously, but not receiving any treatment for osteoporosis (weakening of the bones) that led to this previous fracture. He built this information into his A3 and proposed the creation of a clinic for treating fracture patients with previously untreated osteoporosis. He handed his work over to one of the orthopedic surgeons. We never heard anything about it… until a couple of years later, when the orthopedic surgeon told me that the department had followed the A3 recommendation and set up a Fragility Fracture Clinic that had seen 4,000 patients the previous year. We have had a few examples of lasting impact, and it is very gratifying to see how much the A3 work contributes to the resolution of problems and to energizing our people.
ENHANCING MEDICAL EDUCATION
The rotation is part of our effort to ensure scientific problems solving becomes a bigger part of the education our medical students receive. To further build on this, our team has committed lean coaches to support medical education, rather than just providing a service function. We have also identified two faculty liaison roles – one for the medical school and one for residencies – responsible for the inclusion of quality improvement training in the curricula.
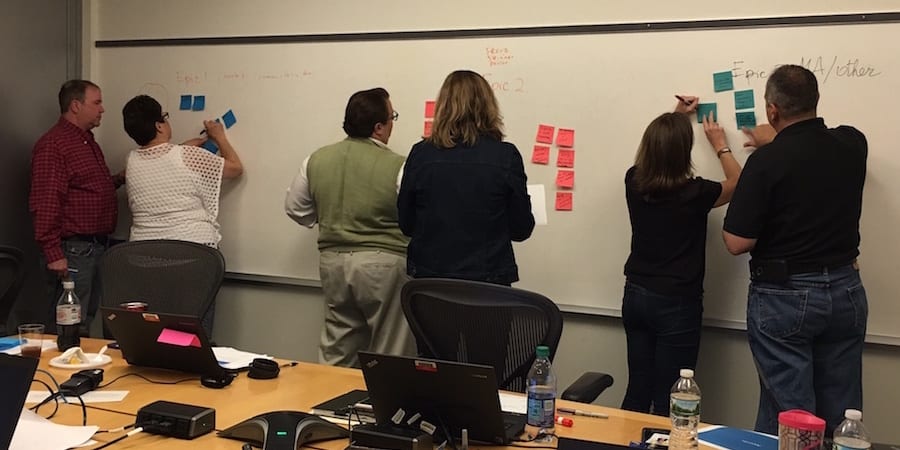
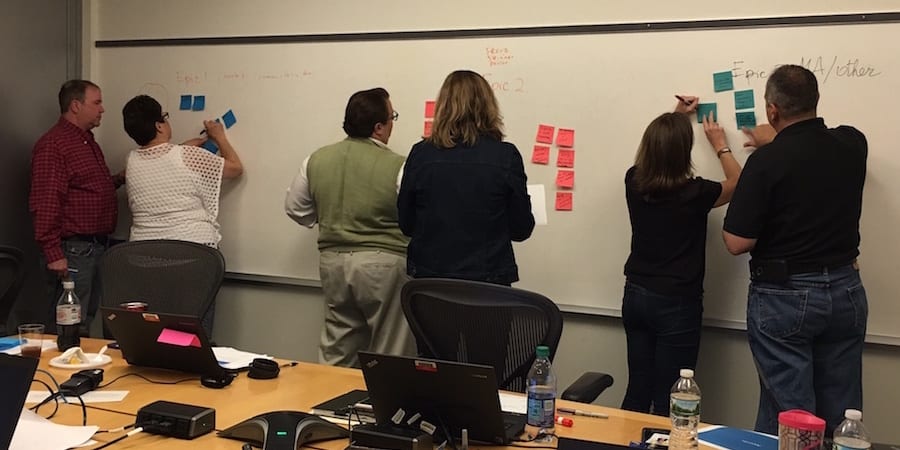
Things are changing. Ten years ago, only a handful of students received A3 training at the University of Michigan Medical School, whereas now all of them are exposed to lean thinking. For the past five years, the entire first year medical school class has had a two-hour A3 exercise – which comprises a 30-minute lecture and then 90 minutes working in small teams on an A3 analyzing a case study of a crowded emergency department. This session now includes dental and nursing students so we will gain experience solving problems across disciplines. And this year, for the first time, all second- and third-year students will also participate in A3 sessions, using real work problems.
Changing the curriculum is a carefully regulated process for the medical school. Part of what broadened A3 adoption was the fact that the University of Michigan was one of 11 medical schools selected for a curriculum redesign program sponsored by the American Medical Association called Accelerating Change in Medical Education. This resulted in an ongoing effort in our school to figure out what and how we should teach students. All the lean seeds we sowed over the years encouraged the curriculum leaders to include scientific problem solving as part of teaching quality improvement and patient safety. When they made their decision, our A3-teaching model was ready for them to use.
We feel a responsibility for our students’ ability to solve problems for the rest of their careers, even though they just spent a month with us. Talk about the Messianic complex that comes with thinking lean!
For a profile on Dr Billi, click here.
THE AUTHOR

Dr. Billi serves as Professor in Internal Medicine and Learning Health Sciences (Medical School), Health Management and Policy (Public Health), and Integrated Systems and Design (Engineering) at the University of Michigan. For the past 13 years, he has led the Michigan Quality System (MQS), the University of Michigan Health System’s (UMHS) business strategy to help transform clinical and administrative operations through development and deployment of scientific problem solving and coaching at all levels.
Read more


THE NAKED GEMBA – Our new series goes back to basics to unlock the secrets of the gemba and tell us about some of the main tools and techniques we can use in a lean transformation. First up, supermarkets.


INTERVIEW – The CIO of a French pharmaceutical company gives us a sneak peek of her presentation at the upcoming Lean IT Summit, focused on using the obeya to change the IT department.


CASE STUDY – To bring consistency to the service provided to customers across their network of workshops, this Brazilian company has turned to Lean Thinking. Along the way, they found in it a different approach to leadership.

INTERVIEW – Business services company Dun & Bradstreet learned that the best way to tackle organizational challenges is using a combination of agile, lean startup and more traditional lean principles.

