
Lean helps save lives in South Africa
FEATURE – Only when we go where the action is, do we begin to truly understand the work. Rose Heathcote joins the Emergency Medical Services in Cape Town for a day.
Words: Rose Heathcote, who took part in the ride along while she was CEO of Lean Institute Africa.
How many of us don’t fully understand the reality of the front line and are genuinely surprised when we get there and take a closer look, busting the myth that we have it all worked out? Going to where the action is and asking curious questions with respect can cure us of our perceptions and pre-conceived ideas. This is a worthwhile lesson to anyone who seeks to support and change things for the better.
I recently spent the day with the Western Cape Government Emergency Medical Services (EMS), including Mercy in the middle and Babie on her right. These are exceptional women.
I’ve seen paramedics and emergency caregivers on TV – exciting stuff! I watch ER, Grey’s Anatomy, Chicago Med and will openly admit to loving Scrubs. Our EMS friends regale us with stories over weekend barbecues. I thought I had a pretty good handle on what it was all about and I’m happy to report I’m on the road to recovery from my naivety.

When I hit the road with the squad, attending to call-outs and witnessing first-hand the real situation, the real people, the real facts and the real challenges they deal with day in and day out, I developed an overwhelming respect for what our emergency care practitioners do for us. Now, when I hear a siren I don’t just nonchalantly look on – I see and feel it differently. That’s the attraction of go see or going to gemba. Your perceptions are altered, your understanding evolves, and you sharpen your skills to support.
Several experiences and observations struck a chord and it’s tough to narrow it down to just a few points. The empathy with which our EMS treat patients and their grieving, traumatized families is a lesson in humanitarianism. Emotions run high and their soothing kindness not only demonstrates a deep respect for people but diffuses some potentially dangerous scenes. Entering the patient’s world and treating them as you would your own friends or family, with caring and humble efficiency.
To put you in the picture, the crew serve some of the toughest areas in Cape Town. Gangsterism, intimidation and poverty are not unusual – some of the people you meet have fallen on hard times and emergency care practitioners have to be both sensitive and alert to do their best in these situations. For example, there is danger of hijacking and leaving valuables in open sight for opportunists is not a good idea. As part of my induction I was asked to remove my jewelry for the day. I did, without argument.
The camaraderie between team members is heart-warming: morning catchups, team spirit and the light-hearted way they embrace and banter before getting down to serious business. They have each other’s backs, and if one of them needs help or protection, the others are there for them.
The unpredictability of the day. Forrest Gump said, “My momma always said life was like a box of chocolates; you never know what you’re gonna get”. That’s how a day in the life for emergency services feels. Yes, you have standard procedures and automatic responses to somewhat repetitive incidents, but you’re dealing with individuals and their unique situations. You have to read the situation and adjust as needed. One size definitely does not fit all.
The EMS value-driven purpose is saving lives. Shifting attention to process for the moment, the basic flow looks as follows:

They are focused on mission time, defined as “from the time a call comes in, until the patient is handed over and ultimately admitted to a healthcare facility” and the emergency care practitioner is free to attend to the next call. This has to be less than an hour.
Challenges impact their ability to meet the mission time, such as call handling times, availability of ambulances, availability of hospital beds, traffic flows, availability of facility staff to receive the patient and opening hours of clinics, to name a few. Even standard procedures can hinder quick response. Ultimately the real flow of the patient journey is from the time someone calls for help until they are discharged from the hospital or clinic (or taking it a step further, until they are ‘healthy’ and fit to leave). It was clear that problems affecting the patient value stream cross borders between hospitals, clinics and the emergency services - and it opens up an opportunity for the various ‘silos’ to gain a common understanding of the issues affecting the entire patient journey, to collaborate and problem solve at the systemic level and gain a healthy respect for the skills each bring to the table.
“The only time we [EMS and Hospital] come to meet is to fight.”
Emergency care practitioners don’t just deal with unpredictability in their day-to-day incidents, but also in patient demand. This fluctuates with the weather (more motor vehicle accidents when it rains), pay-day weekends (more money to spend on entertainment) among other events that trigger incidents. And turning attention to the call center demand, they are plagued by ‘failure demand’ amplified by several calls coming in for the same incident. This, coupled with constrained resources to meet the true demand, puts pressure on the system and could result in calls not attended to in good time, or not attended to at all. Matching capacity to true demand and responding in real time is a critical factor.
I met Babie and her colleagues for the first time at the Lean Institute Africa’s Lean Summit last year. I was quite taken with their enthusiasm and that’s when I asked if I could tag along. I was pleased they were thinking about how they could rethink the way they work, with a view to streamlining how they serve patients and free up resources. I think it is pioneering work in public sector healthcare.
They are learning to tune in to the wastes in their daily work, which sensitizes the squads to the possibilities:
- Time wasted while setting up a vehicle for the day and the way equipment is laid out. Babie explains how 5S helps check and place needed items in the right location to enable quick response times. Every emergency care practitioner has their own way, which makes standardizing difficult. Even zips are lined up for easy access.
- Waiting times affected by incorrect resources dispatched to the scene. Lesser-qualified staff (and patients) wait for the appropriately-qualified employees to arrive.
- Squads are experimenting with reducing set-up time by picking staff up from home and keeping the vehicle running, rather than driving back to base where appropriate.
- Looking at eliminating unnecessary work returning to base to complete a checklist that is actually available on the vehicle MDT (electronic console) and can be completed anywhere.
- Sometimes, internal politics divert attention from delivering value for the patient – and this is not just in EMS. Specialization and disease-centered thinking could corrupt patient-centered thinking. There is a risk of serving metrics, managers and facilities before the patient. We have to ask ourselves who the customer is and what value is in their eyes.
- Call takers receive calls and are driven by the metric to handle the call in under two minutes. The result? In some cases, if they can’t locate where the patient is on the map in good time, and if the patient address is unclear, the crew spends critical time searching for the incident.

While responding to an incident, we were searching for the location and, when we stopped to ask two locals where to go to attend the incident, they simultaneously pointed in different directions!
Waiting time agitates patients and their loved ones. Call handling times may be good, but what is the patient experience? During my go see, patients politely explained how long they’d actually waited. Taking the voice of the patient and extracting the issues is an abundant source of improvement opportunities. And if every squad can be skilled to solve problems every day, in the areas that matter to the patient… the sky is not the limit!
“We want crews to do the situational problem solving, and we want officers to look at trends and systemic problem solving. Solving problems every day at the right level.”
Led by Dr. Heather Tuffin, Mercy and Babie are part of the Revolution Team. This is a relatively new get-up where they’re seconded to deploy a strategic initiative. They aim to bring self-managing squads online in an effort to bring about autonomy to people on the ground. The Revolution Team conducts experiments with their model squad and seeks changes in how patients are serviced – and they are learning to become improvement scientists. What they glean from running experiments with the ‘model’ crew (with the apt name of Ubuntu squad), they intend to deploy to other areas.
“People manage their own homes, so why can’t they manage themselves? We want crews to learn autonomy and self-management. Manage our own paperwork and equipment; analyze our own data and find the gaps to see where we can improve service delivery in our area. Work with the hospitals; build the relationship. Improve work-life balance.”
Squads is a test concept and the team have agreed their value drivers that just so happen to make up the acronym ‘SQUADS’. It helps focus the team to a common goal:
Staff morale - Quality - User experience - Accountability - Delivery - Safety
The Revolution Team has come far in their critical thinking, challenging of assumptions and improvement. They have grappled with problem solving, using a custom-built A3 to guide the thought process and are in the throes of testing several new theories. At the time of writing, they were recruiting five more squads, which is very encouraging as the model cell is now spreading.
“We’ve learned so much about what does and does not work!”
In this way they are learning to think through the issues in a structured way, following cycles of PDSA (Plan-Do-Study-Act) experiments. They are identifying projects to work on, with the intention of developing a new best method for managing squad teams.
“We’ve learned that dealing with people is complex rather than merely complicated. We need to work as a team rather than partners. You have your favorite people, but you have to work with each member of your team, self-managing yourselves. We’ve learned about our team members’ strengths and weaknesses and how to deal with conflict. We realize that it takes a long time for people to start trusting each other – coming from a command and control management style. We want to test if the squad can survive and manage themselves. Arrange their own rosters, service their equipment, improve service delivery and manage their interpersonal issues. We wonder if this is viable?”
The Western Cape Government Health Emergency Medical Services team is two years in and just beginning their lean journey, but it is a solid start. With purpose in hand, clear direction for what must change, cycles of experimentation, a passion for problem solving and the desire to improve service delivery for patients, they are on the road to better things. I cannot wait to see what they achieve in time.
THE AUTHOR

Read more


NOTES FROM THE GEMBA - Two French firms, AIO and Proditec, illustrate how Lean Thinking endures through crises by deliberately developing a new generation of leaders who sustain its culture and intent.


ROUND-UP – In his annual review of the best content we published, our editor looks back at 2022 and what this year was like for the Lean Community.


INTERVIEW – A former VP of Operations from Thales tells Catherine Chabiron how he and his team turned around their department by committing to lean thinking and focusing on people development every day.
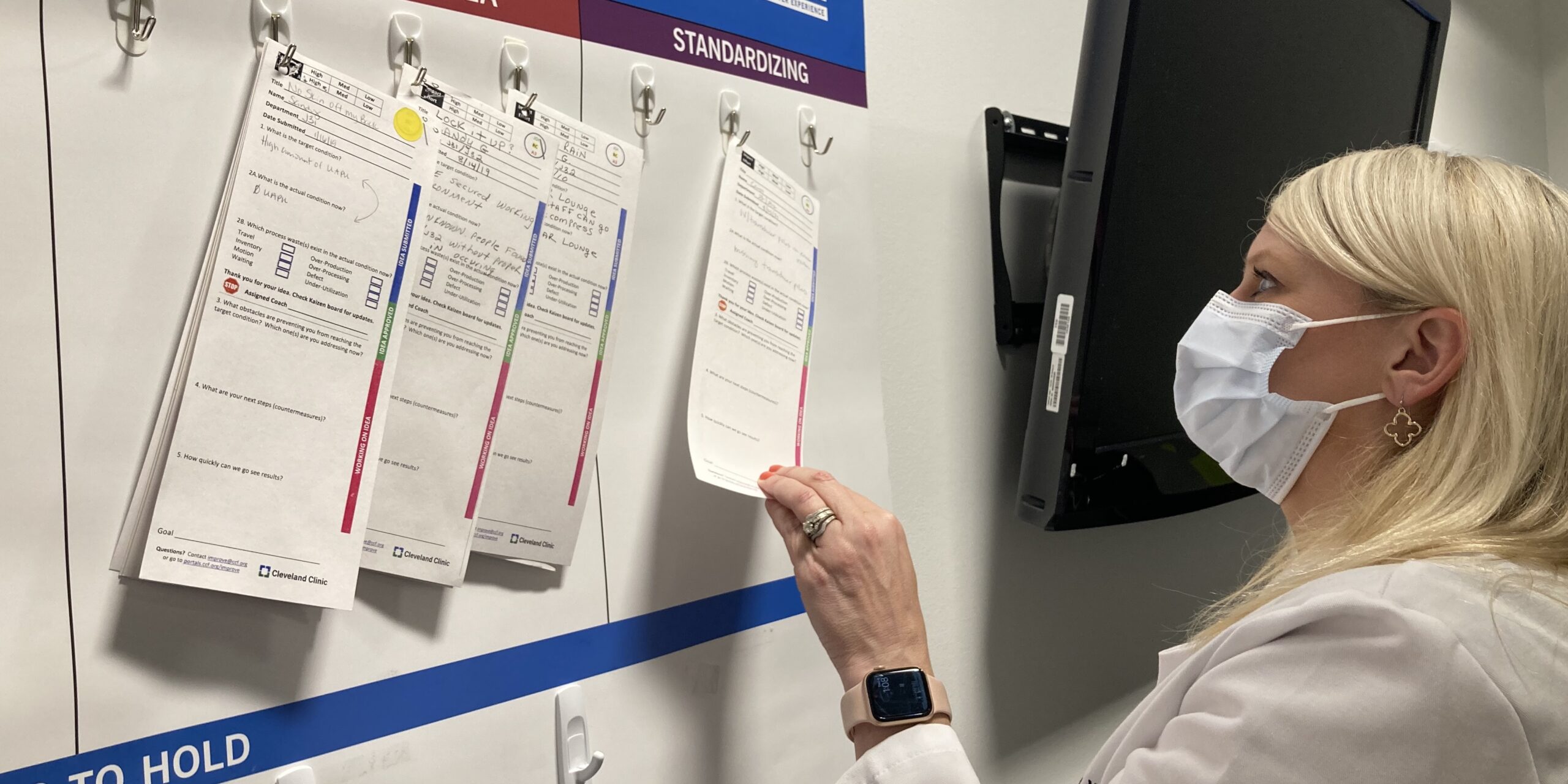

INTERVIEW – Cleveland Clinic has been on a lean journey for a few years now. In this interview, their Chief Improvement Officer and Chief Nursing Officer talk continuous improvement, metrics, and sustaining results.

