
A guide to a system-wide lean healthcare transformation
FEATURE – No healthcare transformation can succeed without a system-wide approach to change. In this article, Dr. John Toussaint, offers his take on the issue, providing a guide for healthcare executives.
Words: John Toussaint, MD, CEO, ThedaCare Center for Healthcare Value
Most attempts at applying lean in healthcare have been superficial. Using tools and doing improvement events is now common, but what is really needed is a system focus: unless the entire organization, from CEO to frontline worker, embraces lean, it’s very unlikely that the few areas that have had successes will sustain their hard-fought gains.
We have a burning platform in healthcare. The industry is responsible for 240,000 to 400,000 deaths per year in the United States due to medical error, according to an article published in the Journal of Patient Safety in 2013. That is a takt time for death of 79 seconds. Many other patients are injured but don’t die. Needless to say, we can - and should - do better.
Healthcare organizations are complex entities, which has led to difficulty in understanding what a complete system transformation looks like. But now, we at ThedaCare have developed a framework for success after years of studying hundreds of different healthcare organizations. Our model defines the key components of successful transformations in healthcare, and it’s no surprise that it starts with leadership.
LEADERS’ PREWORK
Developing a model cell is one of the first actions we encourage, but there is leaders’ prework required.
An organization’s first model cell will be far more personal and emotional for senior leaders than for others. The first step is to recognize that change is necessary, followed by admitting that you need to change. Not just your organization - you. You might need to change only a little. Most of us need to change a lot.
If you pride yourself on your ability to make quick decisions and set people straight, your leadership style is going to need an overhaul. If you have decided that you can delegate the work of change to middle management, you need to adjust that, too. The transformation, therefore, starts with leadership. You will need a sensei, a teacher who can help you to see and learn. That teacher will need to observe you in action at the gemba (where value is created for the patient). You will need to be open to changing your actions and, subsequently, your behavior. You will be required to become a coach and teacher. The new leadership behaviors will be important to support the upcoming work of the model cell.
Also important in this prework stage is that senior executives set the True North for the organization. I don’t mean a broad mission or vision statement, but a number of clear, measurable performance indicators. For example, the Children’s Hospital of Eastern Ontario has established five True North measures, one of which is the number of days patients wait for tests or appointments. True North is critical because the work of the model cell must contribute to True North performance.
CREATE A MODEL CELL
The business case for the first model cell I supported as part of my work helping healthcare organizations embrace lean thinking was “The inpatient experience is disjointed and confusing. The quality results are not reliable, leading to poor customer satisfaction and patient harm.” It focused our team. In 2007 we subsequently went on to create Collaborative Care, the inpatient care model that many hospitals around the world have used as the framework for redesign.
There are five things to focus on when creating the model cell.
1. The model cell must be focused on a business problem that is important to the organization.
2. The model cell runs an inch wide and a mile deep. This means the scope of the project must be limited, usually to one unit or clinic, even though the ideas being tested are intended for the entire organization.
3. Create an entirely new system based on standard work. The team will not be making tweaks or small adjustments to current processes. It will instead create new work processes and will use the scientific method to address any problems that arise.
4. Tie the model cell work to True North. This means, of course, that True North must be established prior to starting the model cell.
5. This work must involve senior leadership. If the work is not championed by a member of the executive leadership, you need to stop and reassess. The hand on the helm must be willing to change, as well.
ESTABLISH PRINCIPLES
The principles lead to systems that eventually drive behaviors. Defining the guiding principles for the organization is very important. My suggestion is that principles should be developed before creating the model cell. The principles can be tested in the real work. Senior leadership should be involved in creating the principles. The Shingo principles are a good place to start the discussion with leadership teams. Leadership teams need to agree on the principles of the transformational operating system. I would suggest not to stray too far from the underlying Shingo framework. In other words, senior teams may choose to change some of the words but should keep the meaning reflected in Transformation house I normally use, which is pictured below. This bedrock allows for the establishment of the next core element, the lean central office.

THE LEAN CENTRAL OFFICE
Think of the improvement team as the bloodstream of an organization. People move through the team acquiring knowledge the way that blood acquires oxygen. These new lean thinkers are then spread through the organization, bringing a specific kind of energy to the front line.
So the purpose of this team is threefold: to facilitate lean activities while teaching lean concepts and to develop the health system’s future leaders. I instituted two-year lean office rotations. Once complete, the facilitators were deployed into management roles. This is the fastest way to change the culture and reduce your need for lean team members. I saw our lean central office begin to shrink on its sixth year because many of our managers were deeply knowledgeable. What I didn’t realize was that we also needed a new management system to support lean.
THE MANAGEMENT SYSTEM
The daily management system is now defined as standardized work at all levels of management to enable a daily dialogue about the most important facts of the business.
It is designed to ensure that everyone is working on the right problems. It is not a set of top-down objectives established on high. In Kim Barnas’ book Beyond Heroes, a lean management system is described as an atmospheric system, where facts on the ground rise like vapor from a lake to mix with the decisions and strategies that fall from above. In the cloud, strategies are informed by facts on the ground, and decisions made at the top are relevant to the front line.
I consider the management system the “secret sauce” of the lean transformation. Changing from the typical top-down Sloan management system to what I term an “improvement” management system is not easy(see my paper “A management, leadership, and board road map to transforming care for patients” on the Spring 2013 issue of Frontiers of Health Services Management).
Again, it requires leaders to change the way they behave. It starts with standard work for calendars and daily activities. The standard work for leaders includes setting True North, prioritizing strategies and deploying the strategy throughout the organization, going to the gemba, visual management, etc.
SPREADING THE WORK
The replication model allows people to learn by doing. This is good. Modular learning enables an entire organization to learn concepts together. This is also good. How to do it is the hard part. Normally, people create training materials for each component, preparing to teach each module across the organization, and go out to spread the good news to the clinics. And that’s where they stumble.
“The problem was we did a tell-and-sell. We went into each clinic and described the model cell and all the benefits they would be getting, and I think the natural human reaction to that is resistance,” James Hereford, who was leading the transformation at Group Health, told me. “So, we heard a lot of reasons why our processes wouldn’t work in that clinic. ‘We’re different,’ people said, or, ‘My patients are different.’ The real problem was that we didn’t ask, we told.”
James’s learning? Allow each spread unit to put their fingerprints all over the work. When we spread model cell work, it wasn’t important to me that each clinic or department had the same standard work. It was important that there was standard work. There is a framework for spread that is nonnegotiable, however. At Thedacare, for example, the model cell clinic found that all lab tests should be drawn at the time of the visit and resulted within 15 minutes. This resulted in fewer callbacks to patients and better quality and patient satisfaction. When spreading to the next clinic, leaders did not tell the team they must use the standard work developed at the Kimberly Clinic (the model cell). Instead, they made it clear that a 15-minute turnaround time was the necessary factor. The spread clinics then used lean thinking to design and test new lab processes to achieve the goal of a 15-minute turnaround time. But without the opportunity to design the standard for the individual clinic, no one at the spread clinics would engage.
This model of spread is not copy and paste. It is copy kaizen. A consequence of this approach is rapid innovation. Michael Erickson, also from Group Health, succeeded James, who left for Stanford to transform that large academic medical center. Instead of only one model cell, now Michael and PAMF have dozens improving standard work every day. Recently, PAMF was ranked by Consumer Reports as having the highest quality in the greater San Francisco Bay Area.
HUMAN DEVELOPMENT
A mistake made by many on the transformation journey is not involving important functions such as HR, finance, and IT.
Let’s examine HR first. HR should be what I saw when touring the Danaher Corporation in 2008. Danaher is a collection of science and technology companies known for being one of the earliest adherents of lean thinking. While walking through their offices, I noticed that just about every workstation had a personal development chart displayed somewhere. It showed the competencies that the person was working to acquire, how long he or she had been on that path, and his or her progress.
It is difficult to describe my reaction to seeing this information, which I thought of as deeply personal, displayed so publicly. I was shocked and a little embarrassed for the person named, yet I could not look away. ThedaCare had something we called personal development goals, but it was a list locked away in our personnel files and usually brought out just once a year during the dreaded annual review. We did not discuss our reviews or our goals publicly. Years later, expectations are now transparent; it is also possible for the individual goals of staff, and progress toward those goals, to be more transparent. This is the piece of the puzzle that I did not yet understand that day at Danaher: when everyone is moving toward common goals, it becomes less personal and judgmental. When caregivers on a unit are trying to incorporate a new technology or care process, ThedaCare is now far more transparent about displaying the names of team members and checking off everyone’s progress toward the goal.
HR needed to learn and practice lean thinking. For example, visual management now extends into the HR department. From a traditional personnel office that closely guarded all information and relied more on sticks than carrots, HR became much more open. The offices now have large, standardized visual management boards. Every job opening and all candidates for positions are posted, as well as each candidate’s progress through interviews and skills assessments.
FINANCE
Finance needed to learn thinking, too. It is time to redefine the true purpose of the finance department as a partner in lean operations, providing expertise in interpreting and translating the numbers. Few finance directors want to be cops, yet that is what our traditional budget processes dictate. Finance is supposed to ride herd on management to assure compliance.
Creating a budget is a major exercise in waste. The moment it is written on paper, it is obsolete. So you spend an entire year trying to reconcile the current reality against what you thought might happen six or nine or 12 months earlier—an exercise that hardly offers new information about the state of your business. Creating a budget causes ongoing fights between managers, who want more resources, and the accountants, who want everyone to stick to seemingly arbitrary numbers. For decades, everyone accepted the discord because the budget process was said to be necessary.
What I imagined for years as CEO was an improvement finance system—a system focused on improving financial performance quarter over quarter. The existing system for most of my tenure was one that simply reset expenses higher each year. The further into the year we went, the more inaccurate the budget was at telling us anything about financial performance. There is a better way. We stumbled across it after reading Jean Cunningham and Orry Fiume’s book Real Numbers in 2005. We learned that an improvement finance system is based on rolling forecasts refreshed every quarter. Tis required us to truly understand our business. That included the real drivers of performance, not 7,000 lines on an Excel spreadsheet. Drivers are the few forces that will make or break a business, such as nursing hours per patient day or number of surgeries per day.
Forecasting is what great lean companies use to improve finances, and it is what we eventually moved to. Forecasting is an estimate of likely future outcomes. It is where leaders think that the organization is heading, adjusted quarterly as new facts emerge. It is a far more accurate gauge of what will happen next quarter—what you will need in terms of resources and the amount of revenue you will likely pull in—and, yet, in every company I know of that has switched to forecasting, it requires less time to prepare.
Thedacare saved 20,000 hours of operation manager and finance staff time by moving to forecasting. Quarterly forecasting takes about 40% the time the obsolete budget system required. All that time has been reinvested back into the operation of the business. Each operations unit has a finance person assigned, which would have been impossible in the budget world.
CLINICAL BUSINESS INTELLIGENCE
When the organization has all the above in place, it still isn’t enough. Healthcare organizations have spent hundreds of billions of dollars on electronic heath records software. The federal government has mandated this. But frontline teams still don’t have meaningful information for improvement. Our goal was to create a system that collects and analyzes data and delivers up-to-date results to frontline clinicians to help them make better decisions and take action. We called the system Clinical Business Intelligence (CBI), and the idea was that people on the front line would use the system to know everything from the current inpatient infection rate to whether units are over- or understaffed. People could then base improvement efforts on current facts rather than hunches or organizational lore.
Today, in more sophisticated organizations such as Salem Health in Oregon, clinicians can access fresh data on the most important activities of clinical care. This information is available simply by clicking on an app, downloading the data, and sharing it. Using this system, they were able to eliminate a life-threatening infection, Clostridium difficile, in the hospital.
TO SUMMARIZE
Learnings from many healthcare organizations around North America have led to the above framework for the lean transformation in healthcare.
This includes establishing a core set of principles to guide the system, committing to personal change as leaders, focusing on creating a model cell addressing a critical need, developing a lean central office with appropriate expertise, and creating a daily management system that includes leaders’ standard work. Learning to spread the model cell work requires supportive administrative functions. These include changes to human development, finance, and IT systems.
Although the transformation may seem like a daunting amount of change, many organizations are plowing ahead and achieving results never imagined. Many of these organizations are participating in the Healthcare Value Network, a learning network designed for leaders to learn share and connect. After visiting many of them, I’m more confident than ever that the lean movement in healthcare is delivering better value care than ever before. There’s a lot left to learn.

JOHN'S NEW BOOK MANAGEMENT ON THE MEND: THE HEALTHCARE EXECUTIVE GUIDE TO SYSTEM TRANSFORMATION WILL BE PUBLISHED IN JUNE. FOR MORE INFORMATION, CLICK HERE.
THE AUTHOR

Read more


FEATURE – Lean provides everyone with a framework to learn continuously and do an ever-better job. Without this understanding, an executive will not be able to steer the organization in the right direction.


FEATURE – Starting off a lean journey is no easy feat, and existing models won’t tell you what the next steps are. That’s why you should go back to basics and let the Toyota Production System “house” from the mid-1980s show you the way.
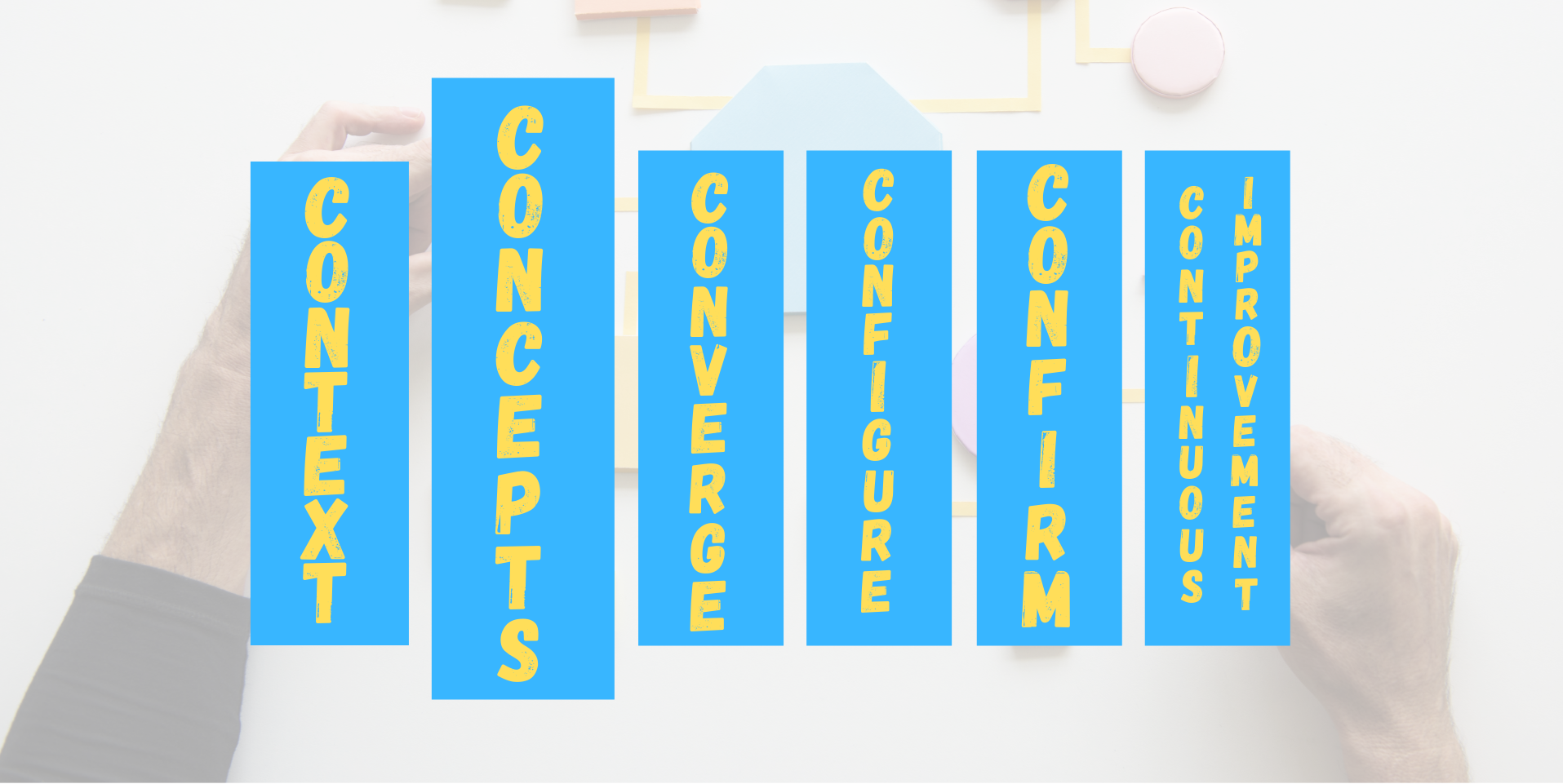

SERIES—The authors discuss Concepts, the second of six elements in their process development model, discovering the key knowledge gaps and exploring multiple process design options to facilitate learning.


SERIES – The authors discuss the fifth of six elements in their 6CON process development model – CONfirm – leveraging a robust launch readiness approach to finalize the process while ensuring it meets the targets set in the business plan.

