
John Toussaint on lean thinking in healthcare
INTERVIEW – At the recent Lean Healthcare Transformation Summit in Brussels, Planet Lean editor Roberto Priolo sat down with John Toussaint to discuss the state of lean thinking in healthcare, its challenges and its opportunities.
Interviewee: John Toussaint, CEO, ThedaCare Center for Healthcare Value and CEO emeritus, ThedaCare
Roberto Priolo: Last October ThedaCare Center for Healthcare Value organized the second Lean Healthcare European Summit. At what stage of adoption of lean thinking in healthcare is Europe compared to North America?
John Toussaint: Europe is seeing early adoption and is probably where North America was five years ago. It will take some time to start to see more mature lean thinking, even though there are already a number of pockets in Europe where lean has really started to take off.
In North America, there are organizations that have been at it for a decade now and we are starting to see pretty sophisticated adoptions of lean there (although we are still far from a Toyota-like ideal state). What matters most is that there are more CEOs in North America now that are good lean thinkers. They are coming into organizations and transforming them from top to bottom. It’s truly great to see.
RP: As a physician yourself, why do you think doctors often find it so difficult to apply the same scientific rigor that they use to diagnose and treat patients to the improvement of processes?
JT: Part of the problem is that we don’t have good scientific evidence around the management system. This has not been studied enough (even though research in this field is starting to appear, in places like HEC Montreal).
We need a specific, in-depth analysis of the different management systems, and at the ThedaCare Center for Healthcare Value we are doing our best to support research in this field. For example, by working with institutions like the Center for Lean Healthcare Research at Fisher College of Business, at Ohio State University.
But even if we don’t have scientific evidence for everything in healthcare, we still need to use continuous improvement principles to build a standard that we can manage and improve over time. This is my argument with clinicians: we might only have evidence for 30% of the things we do, but what about the remaining 70%? We still need a methodology to guide us, and that’s what lean is about.
RP: What were the milestones in the evolution of lean applied to healthcare? Has it followed the same trajectory that lean in manufacturing had?
JT: Yes, and just like with “traditional lean” we have seen a lot of tool-based approaches at first. Since those led nowhere, people hit a wall and started to call us to say, “lean doesn’t work,” when really they just hadn’t done it properly. You need to establish the principles that build the systems that change the behaviors, rather than simply rely on the lean toolbox. It’s all about the management system, which people are starting to understand a little better.
There is more to lean than what consultants generally teach us, and that’s why at the ThedaCare Center for Healthcare Value we have gotten directly involved with a number of CEOs in North America. We are trying to teach that tools are important, but they are not everything.
RP: You recommend creating a model cell as a way to start off your lean efforts in a healthcare organization. How do you decide the area in which that cell lives and what are the key characteristics that such an area must have?
JT: As I explain in my book, you have got to establish criteria to determine where the cell should be created. First of all, there should be a significant business problem that you are trying to solve. If you have a five-hour wait in your Emergency Room, that’s a good place to start.
We want to go where we know there is a lot of pain, so we can really show results. We also need to have our baseline data locked in, so we know how we are performing each day, and then we can do the work on the model cell. This will show people that by redesigning processes we can offer improved care.
The model cell has to be in a place that is really meaningful to the patient. Therefore, it should tackle things like waiting in the ED, or surgical throughput, or infection rates and quality in the medical units. I recommend you start where you have a problem and throw all the resources you have there. Once you start getting results and improving the quality of care for patients, people get engaged.
RP: How would you define a functioning management system that can help a hospital?
JT: Understanding what the strategic objectives are and using hoshin process to ensure everyone in the organization is rowing in the same direction is critical, as is understanding how we are performing at the front line in terms of problem identification and solving.
But I think that even more important is to establish what the roles and responsibilities at each level of management are. Most of the times these have not been clearly defined. And because you don’t know what the standard work for the CEO is versus the standard work for the supervisor at the front line, it all gets jumbled up together and somehow we are all supposed to do the same thing. Every role has a specific set of standards that must be defined, and I haven’t seen enough of that in healthcare.
RP: In your view, what’s the role of a central lean office?
JT: In the first few years of a transformation, I don’t see how you can do it without a central team. In most healthcare organizations, people use different methods of improvement and different ways to measure performance all the time: some are working on Baldrige criteria, others have black belts, and so on. You need to bring that all together into one central office and create a standardized approach to your improvement system.
When you become more established as a lean organization, this is just how you do work and the central office won’t be necessary any more (because at that point everybody has knowledge and there is a process in place to train people). But until you do, you will continue to experience chaos at first without a central lean office.
THE INTERVIEWEE

John Toussaint, MD, is CEO emeritus of ThedaCare and CEO of the ThedaCare Center for Healthcare Value. He was the founding Chair of the Wisconsin Collaborative for Healthcare Quality and of the Wisconsin Health Information Organization, as well as the non-executive leader of the Partnership for Healthcare Payment Reform in Wisconsin. He has been inducted into the Association for Manufacturing Excellence Hall of Fame and been a featured speaker at several international conferences. Dr Toussaint has written three books: On the Mend, Revolutionizing Healthcare to Save Lives and Transform the Industry, winner of the 2012 Shingo Research and Publication Award; Potent Medicine, The Collaborative Cure for Healthcare; and Management on the Mend, The Healthcare Executive Guide to System Transformation.
Read more

BUILDING BRIDGES – Struggling to scale a new product past its MVP phase, Theodo tried a number of things before realizing that the only way to retain quality and speed is kaizen.


FEATURE – We can't go wrong when we trust our people to take the initiative that we will improve their work... that's how Siena University Hospital cut its procurement lead-time in Surgery by two-thirds.


VIDEO - The director of a hotel in the Canary Islands explains the hoshin efforts taking place in the organization and takes us through the lean strategy deployment boards she uses to track progress and highlight problems.
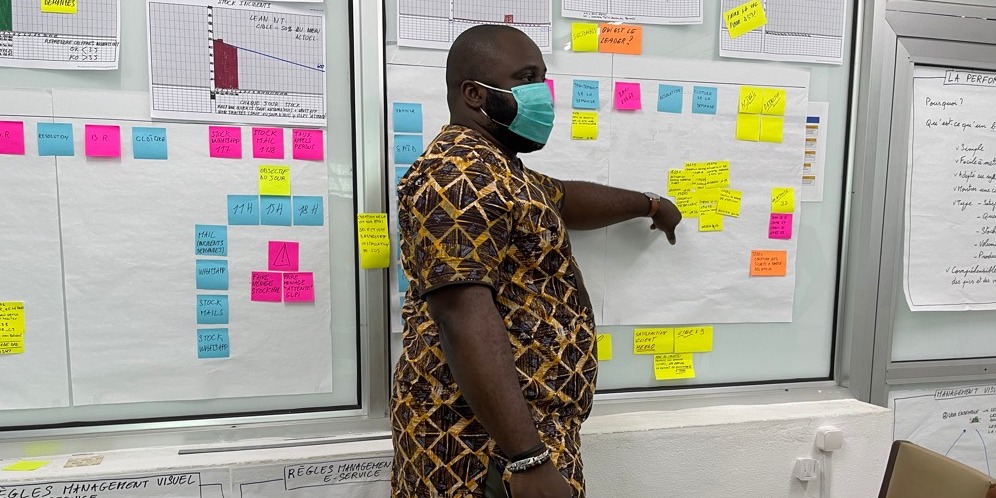

INTERVIEW – In today’s Q&A, we learn how Lean Thinking is supporting the digital transformation of the public administration of the African country of Benin.

